Sunrise strikes again – early hospital discharge is not the problem.
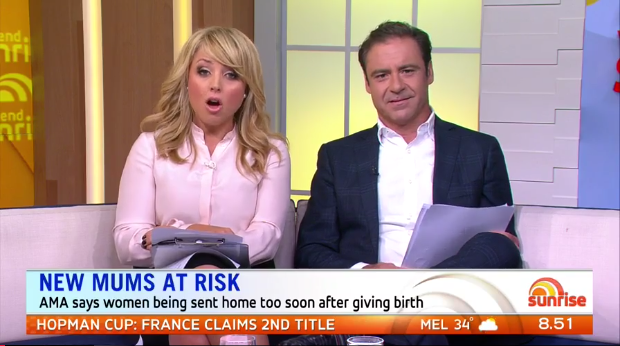
Sunrise co-hosts Monique Wright and Andrew O’Keefe have jumped on the bandwagon yet again (or perhaps more accurately, their producers did) with a story that aired on Channel 7’s Sunrise on January 8th. Click here to watch it.
The segment aired on the back of recent media reports that new mothers are being sent home as early as six hours following birth (obviously referring only healthy women who had normal, uncomplicated labours). Dr Michael Gannon, obstetrician and current President of the Australian Medical Association (AMA) was recently quoted as saying; “as someone who has delivered thousands of babies over the years I have great sympathy and compassion for the difficulties that can occur once returning home.”
This coming from the Perth-based doctor who delivers at a private hospital in Perth that has a 53% Caesarean rate and who still tells his patients who are concerned about lack of fetal movement to “have a cold drink to wake the baby” despite the fact that Perinatal Society of Australia and New Zealand’s guidelines say there is no evidence to support this advice.
Dr Gannon and new mum Codi De Veau were invited to appear on the Sunrise segment and to be honest; I found Dr Gannon’s comments to be pandering, if not downright sanctimonious.
“The majority of my patients in the private sector are very capable, very intelligent, very informed educated women” (Read: wealthy and white).
“But even for people who have the privileges of wealth and the smarts to deal with what might hit them, I feel for them… I know how difficult it is to go home either for the first time or to go home again exhausted after a long pregnancy, maybe a long labour and delivery and have to look after one, two or three other children.”
“I can tell you for sure that assertive patients, well-educated patients, they know the system – they’ll find a way to stay longer but the reality is that there are people in our community who don’t speak English or perhaps don’t speak it so well and in the public system there is no question that we are sending people home who don’t necessarily have the full kit of skills to look after a newborn.”
Really? The “full kit of skills to look after a newborn”? Could he possibly be more patronising?
New mum Codi De Veau then told her story of a long and difficult labour with her daughter that resulted in a Caesarean section. She was sent home after three days, but was struggling with breastfeeding – which is not at all uncommon for Caesarean mothers. It sounds like she was blessed with an amazing midwife, who rang to check on how she was doing and then came to her home with a breast pump from the hospital after he’d finished his shift to help her with expressing her milk. I can’t think of many (any?) obstetricians that would do the same thing.
Andrew O’Keefe seemed stunned that women are being sent home before their milk comes in. He clearly doesn’t know much about breastfeeding (and given Dr Gannon’s response, I wonder if he does either). Women will have a supply of colostrum in their breasts that will more than adequately nourish their newborns for the first few days until their mature breastmilk comes in (usually around Day 3). Again, supply can be adversely affected if a woman had a Caesarean or a highly interventionist labour that involved significant amounts of synthetic hormones, such as Syntocinon, which can lower the release of natural oxytocin for hours (if not days) following birth. Oxytocin plays a key role in the mother-baby dyad of bonding and attachment, which of course is linked to the release of prolactin, the hormone responsible for breast milk synthesis. Even women who had very normal, uncomplicated labours will still go home long before their mature breastmilk comes in.
What this report – and many others – have largely failed to highlight is that the problem doesn’t lie in how long (or short) a period of time a woman stays in hospital postpartum, it’s the support she receives in the days, weeks (and I would argue even MONTHS) following birth. Postpartum support in Australia is abysmal.
The support needs to be AT HOME. Hospital is an artificial environment, making it impossible for mum and baby to settle into any kind of routine for breastfeeding or sleep (especially if she is sharing a room with other women and babies and is constantly interrupted by hospital staff and visitors). She is not eating good nutritious food and her ability to rest and bond with her new baby is severely compromised. Most women are busting to go home!
Professor of midwifery at the University of Western Sydney, Hannah Dahlen, hit the nail on the head when she said keeping women in hospital longer was not the answer. Hospitals did not push new mothers out.
“As long as women get postnatal follow-up at home, then home is the best place for them to be, because their risk of infection is so much lower at home, and you don’t have to listen to the noise of the hospital and have people coming in and out of your hospital room, sometimes offering different advice,” she said.
“It’s not about going home as soon as possible being good or bad, it’s about ensuring women have the best ongoing support once they do get home. That’s where society fails.”
In dramatic contrast, let’s look at Holland where all new mothers are entitled to a kraamverzorger (a professional maternity nurse) for the first eight to ten days after giving birth. The Dutch believe that a mother’s body has a lot of healing to do postpartum while also meeting the near physically exhausting, twenty-four hour demands of a newborn. That’s where a kraamverzorger comes in – to help the mother rest, regain her strength, and bond with her baby in the comfort of her own home.
A kraamverzorger is not only responsible for the well-being of the newborn, but also for closely monitoring a mother’s recovery’s process. It’s a gentle crash course in motherhood where a kraamverzorger serves as an invaluable resource for breastfeeding support, bathing, changing nappies, dressing and feeding. She works closely with a midwife, or an obstetrician if any potential problems arises. An added bonus is that a kraamverzorger can take over household chores – cooking, laundry, tidying up, vacuuming and watching over mum’s other children. Click here to read about one expat mother’s experience of having a kraamverzorger care for her at home.
In Israel, which is where my two children were born, there is a unique and very special community called the African Hebrew Israelites, who predominantly live in the south of the country, in a town called Dimona. When I was studying to be a Lamaze childbirth educator, one of my fellow students was a member of the Hebrew Israelite community and invited our group to visit her amazing community. As a midwife and doula, she helped to run the community’s birth centre.
 Most of the women in the community birthed there (as opposed to having a hospital birth) and they observed a traditional confinement period of at least 40 days following the birth. During that time, the new mother would live at the birth centre where she would rest and recuperate from the birth and bond with her new baby, getting breastfeeding off to a good start. All her meals are cooked for her (a strictly vegan, but delicious and highly nutritious diet – I know from personal experience having eaten there myself!) and she does no cleaning, no household chores and if she has older children at home, they are cared for by other members of the community.
Most of the women in the community birthed there (as opposed to having a hospital birth) and they observed a traditional confinement period of at least 40 days following the birth. During that time, the new mother would live at the birth centre where she would rest and recuperate from the birth and bond with her new baby, getting breastfeeding off to a good start. All her meals are cooked for her (a strictly vegan, but delicious and highly nutritious diet – I know from personal experience having eaten there myself!) and she does no cleaning, no household chores and if she has older children at home, they are cared for by other members of the community.
There are many examples of communities around the world who have postpartum traditions of caring for a new mother. You can read my blog about the Chinese tradition of confinement – or zuò yuè zi, “sitting the month” – here.
If Australian hospitals are so keen to turf women out just hours after birth, why not introduce a government supported national home birth program for healthy, low risk mums along the lines of what women in the UK have through the NHS? Better yet – why can’t we enable women to choose their own care provider and private midwife which they can then claim through Medicare, whether they choose to birth at home or in hospital? Private midwives routinely offer up to six weeks of postpartum support and play a critical role when it comes to picking up breastfeeding problems, perinatal anxiety and postpartum depression.
If we are going to point the finger, let’s point it in the right direction. Keeping women in hospital for longer will not solve the problem. New mothers always have, and always will be nervous and anxious in the early weeks and months. That just comes with the territory of becoming a mother for the first time. The Australian government needs to take a long, hard look at the support it provides new families in those critical early months. The bottom line is, we are doing a terrible job and the record-levels of perinatal anxiety and postpartum depression in this country are proof of that fact.
Tanya Strusberg is the founder of birthwell birthright. She is a Melbourne-based Lamaze Certified Childbirth Educator and a Fellow of the Association of Certified Childbirth Educators (FACCE). She is a passionate advocate for women’s maternity care and her articles have appeared in The Journal of Perinatal Education, Australian Midwifery News, Science & Sensibility, Interaction – the journal of the Childbirth and Parenting Educators Association of Australia (CAPEA), Empowering Birth Magazine, Rockstar Birth Magazine, Mum’s Lounge, Go Ask Mum and Whole Woman. Through her internationally-accredited Lamaze Educator Training program, she is very excited to be training a new generation of Australian Lamaze educators. Last, but absolutely not least, she is also the mum of two beautiful children, her son Liev and daughter Amalia.